May, 2020
New resources answer your questions about PF and COVID-19

“These projects are all part of our effort to help members of our PF community remain informed, supported and connected during the COVID-19 pandemic,” says Sharon Lee, CPFF’s Executive Director. “We are very grateful to the experts appearing in our webinars Dr. Kolb, Ms. Goodwin, Dr. Shapera and Dr. Kalluri for taking the time to speak to our community, when they are exceptionally busy. We also want to thank our sponsors Hoffman-La Roche Ltd. and Boehringer Ingelheim, whose support enabled us to offer these resources so quickly,” says Ms. Lee.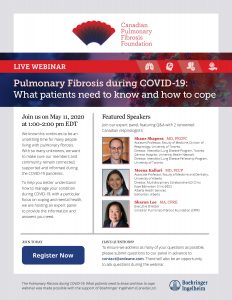
About 275 people participated in the one-hour webinar on April 21 featuring respirologist Dr. Kolb of McMaster University and Sarah Goodwin, ILD Coordinator at St. Joseph’s Healthcare Hamilton, as well as CPFF’s Executive Director Sharon Lee. All three made short presentations, followed by an extensive question and answer session.
You likely have many of the same questions: Are people living with PF more likely to get this coronavirus? Do I still need to go for scheduled breathing and blood tests? If not, will my drug coverage be affected? I’m doing a lot more online shopping. How long does the virus live on packages or envelopes? How do people with PF know they have COVID-19? Will we be treated differently in the hospital emergency department?
These questions, and more, are all addressed in the “Managing Pulmonary Fibrosis During COVID-19” webinar now posted on the CPFF website. You’ll learn more about the virus itself, important precautions you need to take and its impact on PF patients. Ms. Goodwin shares some helpful information about managing your PF in today’s climate of COVID-19, discussing physical activity and pulmonary rehab, mental health and wellbeing and offering some advice for caregivers and family.
You can also register now to participate in our second live webinar, scheduled for May 11 between 1 and 2 p.m. EDT, “Pulmonary Fibrosis during COVID-19: What patients need to know and how to cope.” This webinar will help you better understand how to manage your condition during COVID-19, with a particular focus on coping and mental health. It features two members of CPFF’s Medical Advisory Council, respirologists Dr. Shane Shapera, Director, Interstitial Lung Disease Program, Toronto General Hospital, University Health Network and Dr. Meena Kalluri, Director, Multidisciplinary ILD Clinic, Alberta Health Services, as well as Sharon Lee.
To ensure we address as many of your questions as possible during the webinar, you can submit questions to the panel in advance by emailing [email protected]. There will also be an opportunity to ask questions during the webinar. Don’t worry if you are unable to take part in the webinar during its live presentation. It will be posted on the website, so you can view it at your convenience.
In addition to the webinars, three, five-minute videos, to help people living with PF exercise at home, practice good nutrition and manage stress during the COVID-19 pandemic should also be on the CPFF website shortly.
Along with COVID-19-related webinars and videos, the COVID-19 section on the CPFF website offers many links to reliable sources of COVID-19 and other information, as well as messages from the Foundation.
For more personal connections, some CPFF support groups are meeting virtually and/or their members are keeping in touch by phone, text, or email. Call or email the contact person for the nearest support group to find out how to connect with others. Follow us on Facebook and Twitter to receive notices about new ways to connect and the latest CPFF resources related to COVID-19.
Now, about those questions from the first webinar that we mentioned earlier in this article. Read on for the short answers. For more detailed responses, and much more information, listen to the webinar “Managing Pulmonary Fibrosis During COVID-19.”
- Are people living with PF more likely to get this coronavirus?
There is no evidence that people living with PF are more likely to get COVID-19 than people without PF.
- Do I still need to go for scheduled breathing and blood tests?
Only if your doctor requests that you do so. Most patients will be able to skip one blood test and postpone breathing tests. Provincial governments have waived the need for the breathing tests ordinarily required for continued funding for PF medications for at least the next few months.
- Is it safe for me to go medical appointments or the lab?
Yes. If your doctor needs to see you, every precaution has been made to make your visit to a hospital or clinic safe. Labs have also made many precautions. Appointments can be made online to limit the number of people at the lab at any one time. Employees are gowned, gloved and masked. Some labs provide home visits, but they must be arranged through your doctor and there is a cost involved.
- I’m doing a lot more online shopping. How long does the virus live on packages or envelopes?
The virus lives about 24 hours on packaging. We suggest you empty shipping boxes or envelopes, without touching the contents if possible. Dispose of the box as usual immediately and wash your hands. To be overly cautious, do not touch or use the contents for 72 hours.
- How do people with PF know they have COVID-19? Will we be treated differently in the hospital emergency department?
People with chronic PF do not have the fever, headache or muscle aches that people often have with COVID-19. It is still tricky to distinguish between a flare up, or acute exacerbation of PF, and COVID-19, since some symptoms are the same, such as a cough, fatigue and breathlessness. Just like other patients going to the emergency department, you will be treated as if you do have the virus, until it is determined otherwise. You will be isolated and the staff treating you will take all necessary precautions. You will be tested for COVID-19, with results within six to 24 hours. If you test negative, you will be followed up to determine if you are having an acute exacerbation of your PF.
CPFF awards a record four Robert Davidson Fellowships

The CPFF Board of Directors and Medical Advisory Council is pleased to announce four Robert Davidson Fellowships for the 2020-2021 research period. This is two more fellowships than the Foundation normally funds each year.
“We are able to fund two additional fellowships this year, thanks to generous contributions from two of our sponsors, Boehringer Ingelheim and Hoffman-La Roche Ltd.,” says CPFF Executive Director Sharon Lee.
Each of the fellows are respirologists and will spend at least 75 per cent of their time conducting research and the balance of their time seeing patients, as well as teaching and taking part in the other work in their clinics.
Congratulations to the four new CPFF fellows:

Dr. Colin Adams: Dr. Adams will be supervised by Dr. Shane Shapera. He will perform his clinical work at the ILD clinic at Toronto General Hospital. His primary project will be a Canadian Registry for Pulmonary Fibrosis (CARE-PF) study to develop a new prognostic score for all fibrotic ILD in conjunction with Dr. Jolene Fisher and Dr. Chris Ryerson at UBC. He will also contribute to the Multidisciplinary Interstitial Lung Disease Discussion with Experts Remotely (MILDDER) project, which provides an excellent opportunity for community outreach and facilitating quicker access to care for those living outside the Toronto area.

Dr. Amanda Grant-Orser: Supervised by Drs. Charlene Fell and Kerri Johannson, Dr. Grant-Orser will treat patients at the University of Calgary’s ILD Clinic located at South Health Campus. She will also pursue a Masters in Clinical Epidemiology. Her primary research project during her fellowship will focus on exploring how supplemental oxygen may improve pulmonary exercise hemodynamics in patients with fibrotic ILD and exertional hypoxemia. The ultimate goal of this work is to improve the quality of life and outcomes in patients living with ILD.

Dr. Sarah MacIsaac: Under the supervision of Drs. Nathan Hambly, Martin Kolb and Gerard Cox, Dr. MacIsaac will be working at the ILD clinic at the Firestone Institute for Respiratory Health (FIRH), McMaster University, in Hamilton. She will dedicate 25 per cent of her time providing care to the ILD clinic patients. Her research time will include the completion of a Master’s degree in Public Health, as well as several research projects. Her key research project will be to evaluate the impact of anti-fibrotic treatment on the risk of acute exacerbation following definitive surgical resection or targeted radiation therapy for the management of lung cancer. She’ll also be conducting a quality improvement project to explore measures to expedite access to IPF specialists as well as reduce the interval between the decision to treat and patient receipt of anti-fibrotic therapy.

Dr. Daniel Marinescu: Under the supervision of Dr. Chris Ryerson at UBC, Dr. Marinescu will perform his 20 per cent of clinical duties at St. Paul’s Hospital in Vancouver. While pursuing his Master’s in Health Science at UBC, he will be involved in several research studies. His primary project will examine the association of genetic risk factors with detailed radiological and histopathological findings across various ILD subtypes. The work will serve to better understand the biologic basis for ILD, potentially helping to improve diagnosis and inform effective disease management.
If you are patient at one of the clinics where these new fellows will be working, be sure to welcome them to our PF community.
The Robert Davidson Fellowship supports a one or two-year fellowship in pulmonary fibrosis in Canada with at least 75 per cent of time protected for research-related activities. The combination of clinical and research activities provides candidates with the opportunity for academic career development that will enable them to become key national and international members of the ILD research community. Candidates will be expected to lead a research project at their training institution, with the goal of also participating in multicentre activities that will establish nationwide connections with other Canadian centres.
Making the case for oxygen therapy by surveying experts around the world

Respirologist Dr. Kerri Johannson at the University of Calgary has been advocating for years for improved funding and better access to oxygen therapy for her patients. “Some of my patients are basically suffocating, then I have to subject them to tests to prove they are suffocating, before they can have funding for oxygen therapy in Alberta,” she says.
This restrictive policy for oxygen therapy funding seems to be the result of the limited amount of evidence-based data on the benefits and risks of supplemental oxygen therapy. “There are obvious ethical issues to conducting blinded randomized controlled trials (the highest level of scientific evidence) for oxygen therapy,” she explains. “It’s difficult to ask patients to carry around tanks and tubing and live with the other burdens of oxygen therapy, when they may just be getting room air, rather than oxygen. So creative methods to study this issue are needed”
In light of the limited available evidence, Dr. Johannson led a team of researchers to conduct an international Delphi survey asking 45 chosen ILD experts from 17 countries about their use of oxygen in patients with fibrotic interstitial lung disease to determine which recommendations they could agree upon in using oxygen therapy for people with ILD. The survey questions were derived from a comprehensive literature review and a series of interviews. Survey responders were from countries as diverse as Iceland, Australia, Brazil, Japan, the US and the UK, as well as Canada. Most respondents were physicians; three were nurses; all had expertise in oxygen and ILD.
Published in the European Respiratory Journal in May 2019, “Oxygen in patients with fibrotic interstitial lung disease: an international Delphi survey,” found that the experts agreed that supplemental oxygen should be recommended for patients with fibrotic interstitial lung disease in cases of severe resting hypoxaemia (an abnormally low concentration of oxygen in the blood), or peripheral oxygen saturation <85-89% with exertion, particularly if the patient experienced symptoms due to the hypoxaemia or had to limit their exercise.
The survey also noted that there are differences in funding coverage for oxygen, based on desaturation thresholds, clinical symptoms and testing requirements.
Within Canada there are funding differences for oxygen therapy as well. “Sometimes physicians equate a need for oxygen therapy with what is funded, which is an issue,” says Dr. Johannson. “Just because oxygen is only funded when levels are <80 per cent, doesn’t mean that someone at 82 per cent doesn’t need it, or wouldn’t benefit from it. We should not be making clinical decisions based on funding policies. We need to change funding policy to support the best outcomes and quality of life for our patients.”
Dr. Johannson was also the lead author of an article in the September 2017 issue of the Annals of the American Thoracic Society “Supplemental Oxygen in Interstitial Lung Disease: An Art in Need of Science.” The authors point out that there is limited evidence guiding the use of supplemental oxygen in ILD, and its use varies widely in clinical practice. It is also unclear whether supplemental oxygen improves outcomes and the role of portable oxygen usage for exertion only is particularly controversial.
Unfortunately, in some parts of the country, the lack of robust data creates barriers to funding support and access to supplemental oxygen for patients with ILD. CPFF’s Patient Charter calls for: “Seamless, well-integrated health and social care services, including timely access to ambulatory and personalized home oxygen services and appropriate IPF medications.”
“The absence of evidence is not evidence of absence,” says Dr. Johannson. “We need to influence policy to provide the option to our patients of this vital therapy. We all need oxygen to survive and thrive.”
Oxygen therapy can help patients remain physically active and keep muscles strong, maintaining function and quality of life. Most health professionals agree that activity helps everyone in so many ways, physically, mentally and emotionally.
Further research is needed, but low oxygen levels may increase the risk of pulmonary hypertension, says Dr. Johannson. It is a serious condition characterized by high blood pressure in the arteries to your lungs. The blood vessels that carry blood from your heart to your lungs become hard and narrow and over time, your heart weakens and cannot do its job, resulting in heart failure.
Despite its benefits, both proven and possible, there are some patients who do not want oxygen therapy. They find it a “frightening threshold to cross,” says Dr. Johannson, “thinking it is the first step in their decline. They also don’t want to appear old and sick in public. And it can be difficult to manage for frail patients.”
“It is up to physicians to explain the potential benefits of oxygen therapy and ways it can fit into a patient’s lifestyle and view it as a way to maintain and even improve their quality of life,” she adds. “Ultimately the decision about whether to use oxygen or not is made by the patient, and that decision should be informed by data.”
There is hope that future research into oxygen therapy may lead to a better understanding of its impact on individual’s lives and the health care system. A study in Melbourne, Australia is underway, looking at the rates of hospitalization, quality of life, exercise and deconditioning in people with PF who are on oxygen therapy compared to those who are not. And researchers are looking into ways to use “fitbits” to track activity and study its impacts on the physiology of exercise.
“I hope that the Delphi survey helps to guide physicians in providing oxygen therapy for their ILD patients and helps us to influence funding policy so that this vital therapy remains an option for those who need it,” concludes Dr. Johannson.
Your advance care plan is a gift to your family

On a Monday in late September 2018 Richard “Dick” Martin and his wife Moyra blew bubbles with the Mayor of Calgary to promote public awareness of PF. On Wednesday of the same week, they went to a movie and out to dinner. On Friday morning, Dick was feeling ill and they called an ambulance to take him to the hospital. They remembered to take Dick’s “Green Sleeve” with them. On Sunday, October 1, 2018, Dick passed away.
In Alberta, the Green Sleeve is a plastic pocket containing your advance care planning forms. Think of it like a medical passport. It holds important legal forms that go with you through the healthcare system. In an emergency, Alberta Health Services medical providers can look at your Green Sleeve and know your healthcare wishes.
“With the Green Sleeve, the EMS people knew right away what level of care Dick wanted, and so did the emergency department staff,” says Moyra. “His respirologist Dr. Charlene Fell had completed and signed one of the forms. I was able to focus on supporting my husband and being with him and my sons, rather than making difficult medical decisions.”
Even living with a chronic illness, death can be swift and unexpected. People with PF can experience an acute exacerbation and decline quickly. In these days of COVID-19, more people are thinking about their end-of-life wishes, regardless of their current health.
Advance care planning can spare both you and your family unnecessary additional trauma during the most emotional time – when you are dying. An advance care plan is your personal statement of how medical care choices should be made and who should make them if you become unable to speak for yourself.
You may think that your family can make these decisions for you; that they know what you would want. But, do they? Making these decisions can be very hard on your family, even cause conflict if family members disagree. It’s much easier and less stressful for them – and you – if you state your wishes clearly ahead of time.
There are plenty of online resources to help you through making an advance care plan. The website www.advancecareplanning.ca has plenty of information, tools and workbooks to help you. It also has links to resources and tools from all of Canada’s provinces and territories.
Moyra and Dick worked through Alberta Health Care’s Green Sleeve process together, before calling a family meeting to discuss the decisions they had made. “We told our sons Jeffrey and Gregory that we wanted them to meet with us to discuss their father’s advance care plan. We didn’t want it to be something to discuss during Sunday dinner, but focused on Dick and his wishes and how we could honour them. It really is about trust and communication.”
Be specific about your wishes. Share your feelings and why you’ve made certain decisions. This time can be a chance to share memories, nurture your relationships with others, and say good-bye. If your death happens quickly and unexpectedly, your family may feel assured that you received the medical care you wanted and that you died the way you wanted.
Just bringing up the topic of your eventual death with your loved ones can be difficult. The COVID-19 pandemic may be the opening you need to discuss your wishes with your loved ones and create your own advance care plan to share with them.
Heather and Robert Davidson had an opportunity to talk about an advance care plan when Robert underwent a lung transplant in 2009. “We knew there were risks with the surgery and rejection afterwards, but we chose to focus on a positive outcome, which we were fortunate to experience,” says Heather.
Years later, when Robert went through a series of infections, he brought up advance care planning. “Robert asked me to gather our sons and their wives together to discuss his advance care plans and his wishes,” remembers Heather. “Our sons got quite upset at first, but everyone came to realize that this was not about us, but about what Robert wanted when the time came. It gave us all peace of mind that we were all on the same page.”
As Robert’s health began to deteriorate in 2018, he connected with a palliative care team through his family doctor. They got in touch regularly and he felt free to ask them questions about the end of life and care options. “He wanted to know what it would be like. He looked forward to those discussions,” says Heather. “He could ask what he wanted and get straight answers and he didn’t have to worry about upsetting anyone.”
On April 26, 2019, Robert went into hospital and he passed away while asleep within days on May 1, 2019. “It was a comfort to know that he went the way he wanted to,” says Heather.
Many people avoid discussing advance care planning. Sometimes the patient doesn’t want to discuss it and other times the caregiver doesn’t want to talk about it. It can be a process. Most CPFF support groups will bring in a palliative care specialist to talk to the group. Some members are upset by the topic, others are more receptive. It depends on the individuals, their current condition, their relationships, as well as many other emotional factors.
One spouse of a man living with PF got in touch with a palliative team and found support for herself, when her husband did not want to discuss advance care planning. She discovered she was experiencing “anticipatory grief,” grieving for her husband before he was gone, which was impacting the time they still had together.
Advance care planning can help to alleviate caregiver stress. “It would be good to know that the final care decisions have been made by my husband and I, and communicated to the rest of the family. I worry about the decisions falling to me, at the same time that I am losing my husband.”
Dick Martin, in a video promoting advanced care planning for Alberta Health, left behind some excellent advice for others who may be reluctant to consider advance care planning: “Think beyond yourself and think about your family. And think about the peace of mind and comfort that planning ahead provides.”
Help us continue Robert Davidson’s legacy

There is no doubt that Robert Davidson, CPFF’s late founder would have been the first person to ask how CPFF could help people living with PF during the COVID-19 pandemic. He would then have got to work helping those needing information, reassurance and support in these uncertain times.
May 1, 2020, marks the one-year anniversary of the passing of Robert Davidson, who lived with IPF and established the Canadian Pulmonary Fibrosis Foundation (CPFF) in 2009, less than two years after his own diagnosis and a few months before receiving a double-lung transplant.
He founded the organization to raise funds for research, to provide reliable information to the public, patients and governments and to offer support programs to those affected by pulmonary fibrosis.
Within 10 years, CPFF raised more than $1 million to invest in research, including funding several Robert Davidson clinical fellowships, launched the CPFF website, established support groups across the country, developed a Canadian Patient Charter and successfully advocated for improved access to anti-fibrotic medications in all provinces and territories.
“There is no doubt that CPFF owes its existence to the determination and hard work of Robert,” says Kirk Morrison, Chair of the CPFF Board. “He was an inspiration to so many, including others living with IPF, their families, volunteers and researchers.”
You can help us continue Robert’s legacy of helping Canadians with pulmonary fibrosis, especially during these frightening times. We need your help to provide the virtual resources our vulnerable community needs to stay informed, supported and connected during the COVID-19 pandemic. Please make a donation in Robert’s memory today. He would thank you.


