People with rare diseases deserve equal access to health care

More than 30,000 Canadians are living with pulmonary fibrosis (PF), yet it is considered a rare disease in Canada. February 28 is Rare Disease Day around the world and the Canadian Pulmonary Fibrosis Foundation (CPFF) is joining other rare disease organizations to increase public awareness and advocate for equal access to health care.
Rare diseases affect one in 12 or nearly three million Canadians, but the specialized health care they need, is often difficult to get, or long delayed. Diagnosis is lagging and access to treatment varies across Canada in part due to lack of awareness and understanding of this disease.
Pulmonary Fibrosis kills more than 2,500 Canadians each year, but remains a little-known disease, despite having survival rates lower than many cancers. “If you say the word cancer or diabetes everyone knows what that is. But if you say pulmonary fibrosis, people give you a blank stare and say: ‘What is that?’” says Sharon Lee, Executive Director, CPFF.
Early diagnosis is key
Because it’s a rare disease, pulmonary fibrosis is not top of mind for most family practitioners. The recent 2022 CPFF Patient and Caregiver survey highlights that many patients wait two or more years for a confirmed diagnosis. It’s important to build more awareness so we can shorten that time between a patient experiencing their first symptoms and getting a final diagnosis since most of the medications work by delaying the progression of the disease.
“The sooner we can get a clear diagnosis, the sooner treatments can start, and the more impact can be made in keeping patients stable at a less severe stage of the disease,” says Todd Georgieff, pharmacist and CPFF board member.
Join us for Rare Disease Campaign 2023
CPFF encourages you to reach out to your friends and families to participate in our Rare Disease awareness and fundraising campaign between February 28 and March 31, 2023. In this campaign we salute the courage of those living with the disease and their families, and their determination to work together with CPFF to advocate for improved access to care and to raise funds to invest in PF research. Here are some of the ways you can participate:
- Celebrate a rare individual – send a tribute or memorial card when you make a donation.
- Share the patient and caregiver survey OR the survey highlights.
- Share your PF journey or pay tribute to a rare individual who is living with PF.
- Take the Pucker Up Challenge – People across the country are taking the CPFF Pucker Up Challenge to experience what it feels like to work hard for every breath. Invite friends and family to take the Pucker Up Challenge and help spread the word about PF.
CPFF in the news
As part of our Rare Disease campaign, CPFF has placed an editorial article in the Global Heroes insert in the Globe and Mail and Toronto Star newspapers in Ontario, February 9, and 10, 2023. You can find this article on our website.
Online, we’ll also be celebrating the tenacity, determination and courage of people living with PF by featuring profiles of a few rare individuals. We know there are so many more.
Rare Disease Day is February 28. Take a deep breath, then help support the brave, resilient, and rare individuals living with pulmonary fibrosis. Donate today at www.cpff.ca/raredisease.
cp-news-block
Advocacy Update

Ask your MPP or MLA to Pucker Up
February 28 is Rare Disease Day (see the article above) and as part of our awareness campaign, CPFF is asking provincial elected officials and public servants to take the Pucker Up Challenge to demonstrate their support of CPFF and people living with pulmonary fibrosis.
Once again we’re asking for your help as constituents to reach out to your provincial representative to get involved. Your voice matters. The email message is ready for you to send; all you need to add is your postal code and it will be delivered to your MPP or MLA.
If we all send the message, the impact is substantial. Videos of Pucker Up participation will be amplified through our social media channels. Together we can make a difference!
Patented Medicine Prices Review Board (PMPRB) Guidelines
CPFF is pleased that Health Canada has hit the pause button on proposed new guidelines for the PMPRB and the current guidelines will remain in place until further notice. Health Canada reasoned that “[a] pause will allow time to work collaboratively, with all stakeholders and health system partners, to understand fully the short and long-term impacts of the proposed new Guidelines.” CPFF’s submission to the PMPRB about the proposed new guidelines communicates our concerns as they relate to PF patients.
Government funding for French translation
As a national organization, it is important that CPFF’s materials are provided in both official languages. To that end, CPFF will be applying for government funding for French translation of various materials, including the patient guide, other downloadable resources, web pages, etc.
Upcoming provincial elections
In advance of the Alberta provincial election later this year, representatives of CPFF participated in a webinar hosted by the Health Coalition of Alberta on December 15, 2022 to learn more about the healthcare issues in the province and their relevance to PF patients there. CPFF is seeking to engage with similar health coalitions across the country to monitor provincial-specific issues facing PF patients.
Other provincial elections in 2023:
- Prince Edward Island – October 2, 2023
- Manitoba – October 3, 3023
Webinars
To better understand the global issues and new developments in the field of medicine use and market growth, CPFF attended the IQVIA Institute’s “The Global Use of Medicines 2023” webinar on January 24, 2023.
CPFF fellow advances ILD research and now provides specialist care

Dr. Kelly Sun is a prime example of the goals of the Robert Davidson CPFF Fellowship: to advance knowledge of pulmonary fibrosis (PF) and to train respirologists to expand patient access to PF specialists.
As a 2021-2022 fellowship recipient, Dr. Sun published research on interstitial lung disease (ILD), made a meaningful contribution to the Canadian Registry of Pulmonary Fibrosis (CARE-PF) database, is completing her Master’s degree in clinical epidemiology and secured a position providing ILD specialist care at Credit Valley Hospital in Mississauga, Ontario.
“I am very grateful for the opportunities that the CPFF Fellowship gave me,” says Dr. Sun. “It enabled me to move from Ottawa, pursue new research, advance my academic credentials and hone my clinical skills as an ILD specialist.”
Dr. Sun was the lead investigator of the paper Interstitial Lung Disease in ANCA‑Associated Vasculitis: Pathogenic Considerations and Impact for Patients’ Outcomes published in July 2022 of Current Rheumatology Reports. The review of medical literature, published primarily in the last three years, found that besides immunosuppressive treatments, recent advances in anti-fibrotic therapy may offer patients with progressive AAV-ILD an alternative and/or a more effective and individualized treatment option.
Anti-neutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis (AAV) is a group of autoimmune diseases characterized by inflammation and damage to small blood vessels. Vascular damage in the kidneys and lungs are among the most common manifestations of ANCA vasculitis. Although interstitial lung disease is rare, it can often lead to serious adverse outcomes for those suffering with the condition.
According to Dr. Sun’s study: “[there is] a significant difference in survival between patients with AAV-ILD compared to ANCA vasculitis alone, with 1, 3, and 5-year overall survival rates of 96.7%, 80% and 66% for AAV-ILD .” Importantly, for patients with this type of ILD, and the doctors caring for them, Dr. Sun’s research offers consolidated knowledge of recent studies of AAV-ILD and a new treatment algorithm for the disease. (A treatment algorithm is a diagram used by doctors to help them determine the most effective treatment plan for an individual patient with a certain condition.)
Asked what this research means to patients, physicians and researchers, Dr. Sun, responded: “It offers an updated, succinct summary of a rare disease to promote better understanding for clinicians and researchers, who are then better able to treat patients and continue to build upon current knowledge.” She adds that the new treatment algorithm should be helpful for those clinicians who may be less familiar with the disease or feel the treatment of this severe, rare illness is quite daunting.
In addition to this paper, Dr. Sun added about 100 patient records to the CARE-PF database, a Canada-wide, multicentre, patient registry. Each record involved many hours of review with other members of the multi-disciplinary team at the ILD Clinic at Toronto General Hospital, part of the University Health Network (UHN). The CARE-PF database is used by researchers across the country to better understand the biologic basis for ILD, helping to improve diagnosis and inform effective disease management.
Dr. Sun was also a contributor to an ongoing study spearheaded by her Toronto colleagues on unclassifiable ILD. The study is analyzing radiographic and clinical patterns to help determine diagnosis and develop treatment approaches for those suffering from unclassifiable disease.
During her fellowship year, Dr. Sun also cared for patients at the ILD clinic, took part in a variety of multi-disciplinary rounds and taught monthly sessions to residents rotating through respirology.
With this fellowship, Dr. Sun says she was able to train in a world-class ILD centre, gain clinical knowledge to better serve patients with ILD and complex needs, and foster lifelong connections with mentors, specialists and researchers in a variety of disciplines, from across the country.
“I want to thank all the donors and sponsors of the CPFF that support the Robert Davidson Fellowship program,” says Dr Sun. “I am now exceptionally prepared to provide the best care possible to my patients and to continue to contribute to research in the field.”
Name the CPFF mascot
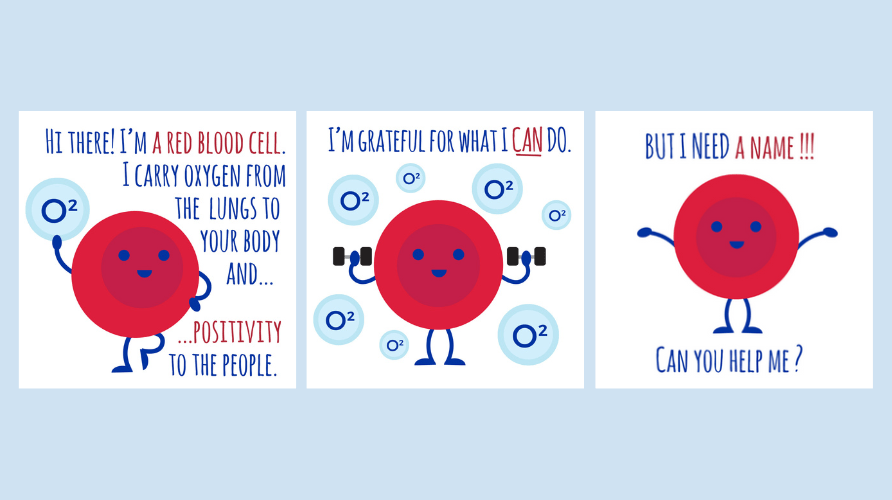
The CPFF community has experienced the incredible strength of people living with pulmonary fibrosis. Many of these courageous individuals showcase hope despite the energy it takes to live with this devastating disease. CPFF has decided to create a mascot that will share some of this positivity with the rest of the community.
Our mascot needs a name. Any ideas? Click this link to submit your name idea.
Submit your name idea by February 24, 2023. The final name will be announced in early March on social media, in the CPFF app, and in this newsletter.
Webinar series helps you understand and deal with the role of mast cells in PF
Tracey Reed brings a welcoming smile, lots of science-based information, easy-to-follow tips and a positive outlook to her audience. Following a well-received webinar last September on an anti-inflammatory diet for pulmonary fibrosis (PF), the holistic nutritional consultant agreed to deliver a three-part series of webinars that looks more closely at the role of mast cells in the development of PF.
In her down-to-earth fashion, she gives you concrete examples of the lifestyle changes, both in your diet and in other ways, that can help you stabilize your mast cells, which may slow the progression of fibrosis.
All three webinars are now available for viewing on cpff.ca, in the video library at your convenience:
- Mast cells in PF, Nov. 10, 2022
- Dietary strategies to stabilize mast cells, Dec. 8, 2022
- Other lifestyle strategies to stabilize mast cells, Jan. 12, 2023
In the first session, she looks at the role of mast cells in the body, what happens when they go awry, what the research tells us about mast cells in PF and other signs and symptoms.
Mast cells are a type of immune cell that regulate many functions in the body, including getting rid of unwanted bacteria and parasites. They are also communicator cells, signaling to other immune cells to get to work.
Mast cells have over 1000 chemical mediators that they can selectively release to signal different actions in cells throughout the body. These mast cell mediators attract leukocytes to amplify inflammation.
Mast cells are found in: the skin, gut, lungs and sinuses, bladder, reproductive tracts, blood vessels and the blood brain barrier. They are multifunctional, ensuring the integrity and permeability of certain tissues, immune regulation, microbial defense against bacteria, viruses and parasites, and in wound repair.
The most well-known mast cell response is allergies. During an allergic reaction, the antigen binds to antibodies on mast cell receptors. Histamine and other chemical mediators are released, inducing allergic symptoms.
Lung tissue has more mast cells than other tissues in the body and an accumulation of these cells is found in fibrosis. Mast cells release chemicals initiating collagen fibril formation. When collagen production happens faster than collagen breakdown, you get an accumulation of fibrillar collagen, or fibrosis. The anti-fibrotic medications ninetanib and pirfenidone interfere with the release of mast cell chemicals to reduce the build up of fibrosis.

Part 2: Dietary strategies to stabilize mast cells
In this session, Reed focuses on histamine and what you need to know about it. She outlines how to reduce histamine triggers and explains some real-life tips on how to incorporate dietary changes to stabilize mast cells.
Histamine is a “signal” that can bind to mast cell receptors and signal the release of chemical mediators involved in PF. It is found in the body, stored in mast cells; produced by gut microbes; and in food. Histamine is cleared from the body with two enzymes (DAO and HNMT).
“What we want to achieve is to keep a balance between the histamine “in” and histamine “out,” says Reed. She calls this the HIHO, or histamine in, histamine out, principle.
Reed talks the audience through three tips to get started reducing the amount of histamine in your diet:
- eat fresh
- freeze leftovers
- replace foods high in histamine with substitutes.
Eating fresh means finding the freshest produce you can. In season and local is best with frozen fruits and vegetables being another great choice. As for fresh meat, check the dates – best before and/or packaged on.
After cooking, histamine in foods increases quickly, especially in meats. Reed suggests individually portioning leftovers as soon as possible and freezing them. Individual portions offer more flexibility and thaw quicker when needed.
Reed also offers a list of high-histamine foods to avoid and offers possible replacements for some of them.
On the other side of the equation, she offers options for foods containing nutrients that help stabilize mast cells, reducing the amount of histamine they release. For example pea shoots have the DAO enzyme. She also offers lists of foods with quercetin and vitamin C that help stabilize mast cells.
In a practical vein, Reed also provides tips for getting the most bang for your buck when buying food, such as buying in bulk and freezing the excess. Another tip refers to the “Clean Fifteen” and the “Dirty Dozen,” two lists produced by the Environmental Working Group of the best and worst of produce in terms of chemical residue.
A final tip involves having half of your plate, bowl, or smoothie, consist of low histamine fruits and vegetables at every meal to get the quercetin and vitamin C you need to stabilize mast cells. As suggested by the latest Canada Food Guide, another quarter of the meal should be plant or animal protein and the final quarter with whole grains or other carbohydrates. Reed recommends adding healthy fats as well, such as olive oil, ghee, or avocado oil.
To complete this session, Reed has added a recipe and a cooking video.
Part 3: Other lifestyle strategies to stabilize mast cells
This third and last webinar by Tracey Reed focuses on other lifestyle strategies to stabilize mast cells.
To avoid triggering mast cells in the lungs, avoiding injury to the lungs is key. The list of lung injury triggers include:
- Mining (coal dust, metal dust)
- Farming (Roundup, grain dust)
- Construction (asbestos)
- Exposure to toxins or pollutants (mold, smoking, radiation, some medications)
- Disease (connective tissue autoimmune diseases)
- Infections (Epstein-Barr, Herpes virus 8, Lyme disease)
Mast cells can also be triggered by:
- Foods
- Stress (current or past)
- Exercise
- Temperature extremes or changes
- Physical stimuli
- Toxins
- EMFs (electromagnetic fields)
- Hormones
- Infection
- Hypoxia (inadequate oxygen)
The link between neurons, or nerve cells and mast cells often give rise to overactive mast cells. Neurons like to hang out with mast cells, and mast cells like to hang out with neurons. Mast cells can travel, and they will travel to be close to nerves, as well as to barrier tissue such as your skin, your sinuses and lungs, your gut and your bladder.
When triggered, by lung injury or other triggers, mast cells say: Ramp things up! More inflammation. More pain! And nerve cells say: Keep talking! Tell me more! In this way, neurons and mast cells prime or sensitize one another. Neurons communicate in the language of neuropeptides and nerve growth factors. Mast cells communicate with mediators such as histamine, interleukins, growth factors and others. Many of these are pro-fibrotic.
This cross talk between neurons and mast cells starts with:
- Injury or physical trauma
- Infection
- Toxins or pollutants
- Other disease states
- Anything that doesn’t feel safe in the body
How can you stop the cross talk between neurons and mast cells? Practices such as yoga, meditation and mindfulness help to calm the nervous system, quieting the nerve cells’ response. Anything that relaxes you and your nervous system can help. A warm bath with Epsom salts. Open up your windows and doors and let fresh air move through your home for short time. Even in winter (on a milder day), fresh air helps remove air-borne irritants that may be trapped indoors.
Tracey also noted a couple of free apps for meditation sessions: Insight Timer and OAK, which is especially good for beginners.
And as noted in Reed’s Part 2 webinar, dietary strategies can help inhibit mast cell activation and make mast cells more stable. When this happens, your mast cells stop releasing the chemicals that sensitize your nerves.
At the end of each webinar, Tracey Reed shares her contact information for those who would like to follow-up with her holistic nutritional practice.
- Website: histaminehaven.com
- Email: [email protected]
- Visit histaminehaven.com/courses to find First Steps
George Kaminsky was a great support to others facing PF

The Board of CPFF is saddened to share the news that former Board member George Kaminsky passed away on December 11, 2022. He served on the Board for several years until 2019 and was involved for many years with the Vancouver PF Support Group. He was 72 years old.
Almost 10 full years after a double-lung transplant, his new lungs remained well and healthy, but his heart did not, says his wife Joy. After 48 hours at Lions Gate Hospital, he passed away peacefully.
Many have written to Joy via Facebook about how helpful George was to them when they first got their diagnosis; explaining to them what would happen next and where they could find support and information – at CPFF. He would have been so pleased to read their comments, as he wanted to help others as he had been helped, says Joy. He hated giving up on his involvement with CPFF and the Support Group, but he had to focus on his health.
George told his doctors just two days before he passed away that his happiest moments were seeing his grandsons Keanu and Locke, and that he had lived long enough to see his sons Julian and Joel grow into wonderful men. And, he still really wanted to pick up a golf club and swing it again!
We extend our heartfelt condolences to George’s wife Joy and his sons and all of his family and friends. A celebration of George’s life was held last weekend. He will be missed.
My journey with IPF

Submitted by Dale Smith
In 2009 I had lung cancer and had my upper left lobe removed on my 50th birthday. I recovered well and was back to work within weeks. About a year later, I started having shortness of breath, coughing, and had trouble getting through a day of work.
After a lung biopsy and months of testing for this and that, and everything in between, I was diagnosed with IPF, given some literature and told the average life expectancy was five years.
I did my follow ups with respirologists for several years with no real disease progression and then in early 2020 things started progressing. I was then put on oxygen and OFEV in December 2020. At this time there was finally talk of lung transplant.

The first thing I needed to do was drop some weight. I began a long, hard struggle with the 100 plus pounds I was over, to meet the criteria. I decided I was up for the challenge. It was either that or lay down and die. I wasn’t about to do that, so I walked and walked, and walked some more. I gave up all my comfort foods and traded them for salads and veggies. My grandkids gave me lots of inspiration to make this lung transplant happen. I need to be here when they graduate!
By September 2021, I had dropped 120 lbs. Next was dozens of tests for the transplant and finally by July 2022 I met all the criteria and was placed on the transplant list. I sit here now waiting for “my call,” waiting for someone to give me life with the donation of their organs at the end of their life.
The doctors have said transplant is not a cure, just a trade off for other ailments and diseases, but at this point it’s a trade I am willing to make. With my 60th birthday right around the corner, and ten years into this journey, I am still here. And I am confident that I will get my second chance and still be here ten years from now!



